The historical foundation that produced the concepts of mind and body can be traced back to the ancient Greek frameworks of Aristotle and Plato. Plato believed the body and soul are two separate entities and mastered the understanding of the soul. On the contrary, Aristotle believed that the two entities are intertwined and belong together in which one cannot exist optimally without the other [1], and focused his understanding mainly in the mind. Although these two are separate and contradicting theories, they both agree that the mind is the connection between the body and the soul.

A seventeenth-century French philosopher figure Rene Descartes theorized the distinction between the mind and the body, where it was not unusual to view the “mind” separately from the “body.” The differentiation was that the mind was seen as the concern of organized religion, while the body was seen as the concern of physicians[1]. This served the preeminent principle in a separation between the so-called “mental” and “physical” health. With advancement in technology, the twentieth century has recognized remarkable development in the understanding of mental disorders and the brains. There is a growing realization of the centrality of mental health to overall health and well-being.

The mind and the body not only influence each other, they are each other.
As Socrates says in the Lesser Hippias, “You will do me much greater benefit if you were to cure my soul of ignorance, than you would if you were to cure my body of disease[1].”
- Mind and body are certainly connected. How? Well, think about what happens when you become ill, and for this instance you came down with a flu. You run a high fever and feel as if your whole body is breaking in half, not only your body, but your mind doesn’t seem to work as well. When having a flu, it’s advised to rest as much as possible, increase fluid intake and consume light food in order to feel better.
- Now, think about going to work or school or doing any activities when you are in this state. You would be lucky if you did not pass out, but others around you would not be as lucky as you as their chances of catching the flu have increased. Besides, you could have ended up in the hospital for extended care when you have exerted too much of your body when it needs extra rest, not extra work.
- This is very similar to mental health problems, for example you are diagnosed with depression. The only thing you would want to do is to rest and not physically do anything. But that’s not the right way to self-care. Self-care in this case would be to see a licensed therapist, take your prescribed medication, and follow the treatment plan or engage in physical activity.
- A well-balanced lifestyle helps eliminate unnecessary mental and health problems. Taking care of oneself by allowing yourself to get a good night sleep, eat healthy meals, exercise regularly, follow treatment plans (if any) and take medications as told will help you be ready to tackle life, and stay both physically and mentally healthy.
- You can think of it as if you are working out in the gym. If you only focus on one of your muscles, let’s say your bicep. Yes, you would have strong biceps, but what about your other muscles? If you only work on one muscle, you would only have one strong muscle. At the same time, you could focus on all your muscles equally and have a stronger body instead of just one stronger muscle.
When dealing with any psychiatric or medical disorders, exercise is most definitely the last thing on your to-do list. Interesting enough, exercise should be one of the things that belong on top of your to-do list. There are many benefits from engaging in physical activities. But before we go into the good stuff, allow me to explain why you should squeeze in exercising time in your busy schedule.
Everyone knows regular exercise is beneficial to the body and it helps trim that waistline, cut down the extra pounds, and build that abs that you have always dreamt of. BUT, did you know that exercise is also one of the most effective methods to improve mental health? And no, exercising does not mean only to go to the gym and run on treadmill or lift heavy weights. Any physical activities such as gardening, walking around the block with your lovely pets, using stairs instead of elevator or simply engaging in other less intense activities are considered exercise. All in all, pretty much anything that gets you off the couch. Impact of exercise on mental health is underrated, but benefits of physical activity on mental health are quite extensive.
Regular exercise can have a profoundly positive impact on mental disorders including depression, anxiety, ADHD etc[4]. It can relieve stress, improves memory, helps with sleep, and boosts overall mood. Exercise is not always about the muscle size and aerobic capacity. It gives an enormous sense of well-being and healthy living.

Stress relief
- When you are under stress, your body begins to give a different feel from when you are in normal state. Your muscles become tense, especially in the face, neck and shoulders areas, leading to back or neck pain and painful headaches. You may also feel a tightness in your chest, a pounding pulse, or muscle cramps. With stress, it is possible to experience insomnia, heartburn, stomachache, diarrhea and such. The discomforts and worries can eventually lead to chronic depression and the continual of the cycle.[4]
- Exercise is a great natural stress relief and an effective way to break this vicious cycle. During exercise, your body releases a chemical called endorphins. Endorphins interact with the receptors in your brain that reduce your perception of pain and stress[4]. They also trigger a positive feeling in the body.
- In a study done by James Blumenthal, PhD, a clinical psychologist at Duke University, Blumenthal and his colleagues assigned sedentary adults with major depressive disorder to one of the four groups: supervised exercise, home-based exercise, antidepressant therapy, and a placebo pill.
- After four months of treatment, Blumenthal found that patients in the exercise and antidepressant groups had higher rates of remission than did the patients on the placebo.
- He concluded that exercise was generally comparable to antidepressants for patients with major depressive disorder.
- Blumenthal followed up with the patients one year later. The type of treatment they received during the four-month trial didn’t predict remission a year later.
- However, subjects who reported regular exercise at the one-year follow-up had lower depression scores than did their less active counterparts. In which he said, “Exercise seems not only important for treating depression, but also in preventing relapse.”[4]
Boost your happiness and lower anxiety
- As well as reducing the perception of pain and stress, endorphins create feelings of happiness and euphoria. Following a run or workout, many often described the feeling as “euphoric.” This feeling is known as a “runner’s high,” because they are accompanied by a positive and energizing outlook on life[5]. With that being said, exercise can alleviate symptoms of depression or anxiety. Instead of depending on medication, exercise can be your effective (and natural) antidepressant pills.
- When we are spooked or threatened, our nervous system jumps into action, setting off a cascade of reactions such as sweating, dizziness, and a racing heart. People with heightened sensitivity to anxiety respond to those sensations with fear[5]. They are also more likely to develop panic disorder down the road, according to Jasper Smits, PhD, Co-Director of the Anxiety Research and Treatment Program at Southern Methodist University.
- Smits suggested that regular workouts might help people prone to anxiety become less likely to panic when they experience those fight-or-flight sensations.
- After all, the body produces many of the same physical reactions in response to exercise.
- They tested their theory among 60 volunteers with heightened sensitivity to anxiety.
- Subjects who participated in a two-week exercise program showed significant improvements in anxiety sensitivity compared with a control group.
- People learn to associate the symptoms with safety instead of danger.
- The findings suggest that physical exercise could help to ward off panic attacks[5].
Reduce ADHD
- Studies have shown that regular exercise improve concentration, motivation, memory, and mood.
- Exercising boosts the brain released of dopamine, norepinephrine, and serotonin levels –in all of which affect focus and attention.
- More specifically, getting sweaty increases production of cells in hippocampus responsible for memory and learning[6].
- Because of this, exercise can be a replacement of Ritalin and Adderall medications.
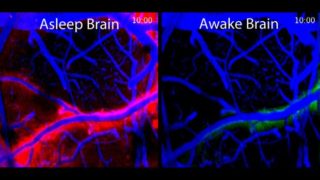
Prevent cognitive decline — Dementia and Alzheimer’s
- Truth hurts, but as we get older, our brains get a little fuzzy. As aging and degenerative diseases like Alzheimer’s kill of brain cells, the noggin actually shrinks, losing many important brain functions in the process[7]. While exercise cannot cure the disease, it can help the brain slow down the cognitive decline.
- Levels of the essential nutrient, choline, rise with an increased loss of nerve cells – a marker of Alzheimer’s disease.
- Last year, researchers at Goethe University Frankfurt had senior volunteers (aged 65-85) ride a stationary bicycle three times a week for thirty minutes over a twelve-week period; the control group did not exercise.
- The exercising group experienced stabilized choline levels, while the control saw an increase in this metabolite[7].
- Another study from 2013 stresses the importance of cardiovascular exercise. Art Kramer, a neuroscientist who directs the University of Illinois’s Beckman Institute for Advanced Science and Technology, directed one group of older adults to exercise moderately for 45 mins, three times a week.
- The control group ended up losing 1.5 percent of brain volume, while the exercising group increased brain volume by 2 percent[7]. This increased volume resulted in better memory scores.
Build self-confidence
- Physical activity can boost self-esteem and improve positive self-image.
- Regardless of weight, size, gender, or age, exercise can quickly elevate a person’s perception of his or her attractiveness, that is, self-worth[8].
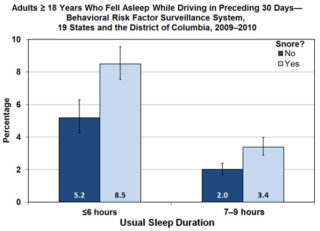
Lastly, the most obvious reason: better sleep!
- After running 30 minutes on treadmill or a session of any kind of exercising, your body feels relaxed.
- A moderate workout can be the equivalent of a sleeping pill, ever for people with insomnia[5].
- Physical activity raises the body’s core temperature. When the body temperature drops back to normal, it signals the body that it’s time to sleep!
- Exercise promotes better sleep.
[1] Burton, N., M.D. (2010, March). Plato and Aristotle on health and disease. Psychology Today. Retrieved from https://www.psychologytoday.com/us/blog/hide-and-seek/201203/plato-and-aristotle-health-and-disease
[2] Connection Between Mental and Physical Health. (n.d.). Retrieved from http://ontario.cmha.ca/documents/connection-between-mental-and-physical-health/)
[3] Weinberg, J., M.D. (2018, Feb). Mind-Body Connection: Understanding the Psycho-Emotional Roots of Disease. Retrieved from https://chopra.com/articles/mind-body-connection-understanding-the-psycho-emotional-roots-of-disease
[4] Bhandari, S., MD. (2018, February 21). Exercise and Depression. Retrieved from https://www.webmd.com/depression/exercise-depression
[5] Breene, S. (2013, October 7). 13 Unexpected Benefits of Exercise. Retrieved from https://greatist.com/fitness/13-awesome-mental-health-benefits-exercise
[6] Robinson, L., Segal, J., Ph.D, & Smith, M. (2018, March). The Mental Health Benefits of Exercise. Retrieved from https://www.helpguide.org/articles/healthy-living/the-mental-health-benefits-of-exercise.htm
[7] Beres, D. (2018, February 27). Can exercise prevent dementia? Retrieved from http://bigthink.com/21st-century-spirituality/does-lack-of-exercise-lead-to-dementia
[8] Weir, K. (2011, December). The Exercise Effect. American Psychological Association. Retrieved from http://www.apa.org/monitor/2011/12/exercise.aspx